Patient concerns over ever-increasing costs are growing, especially when it comes to their health care. Morning Consult recently conducted a 50-state poll of 20,000 Americans on behalf of PhRMA to get to the root of affordability challenges, and to learn more about what real people believe policymakers should do to tackle these problems.
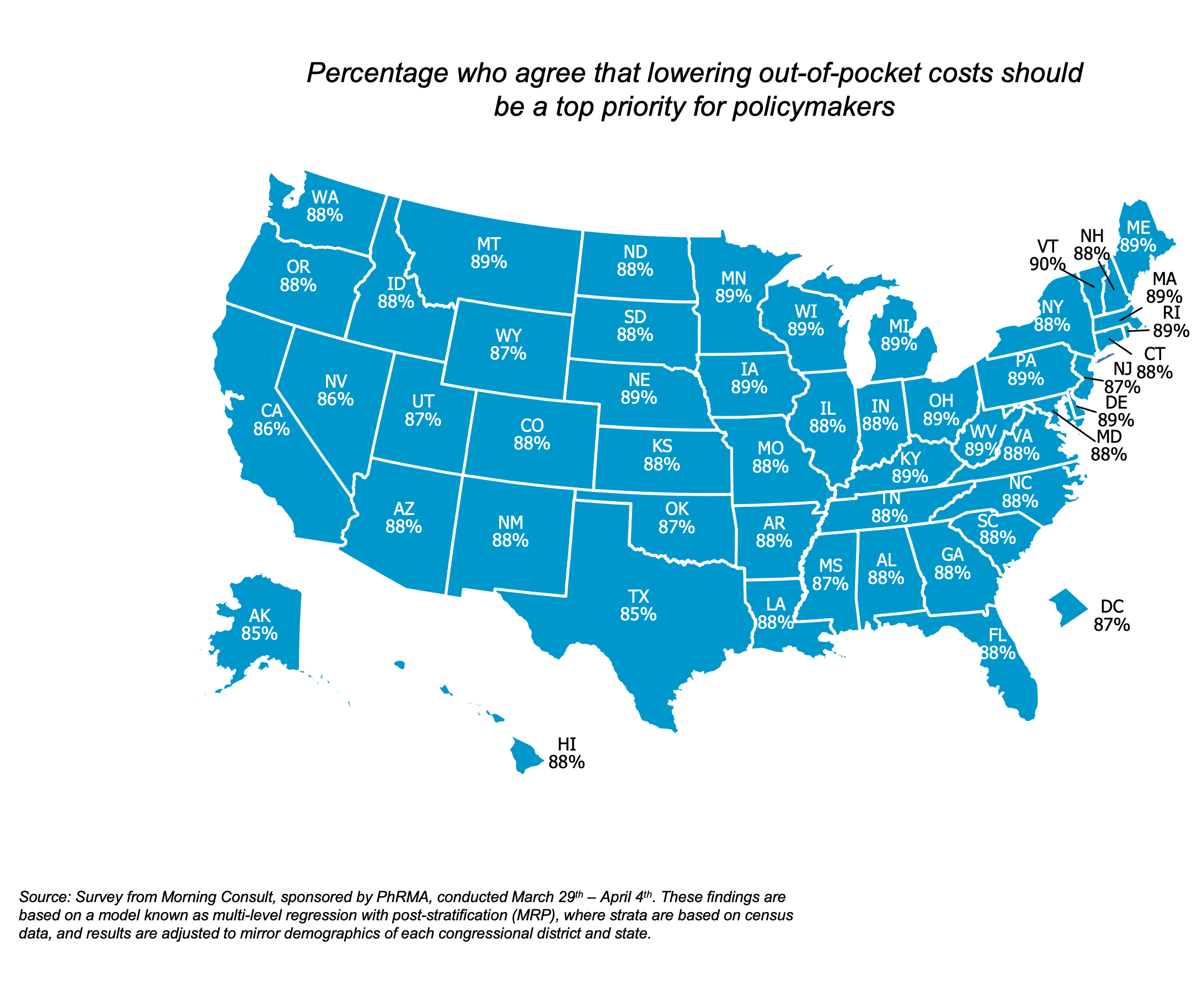
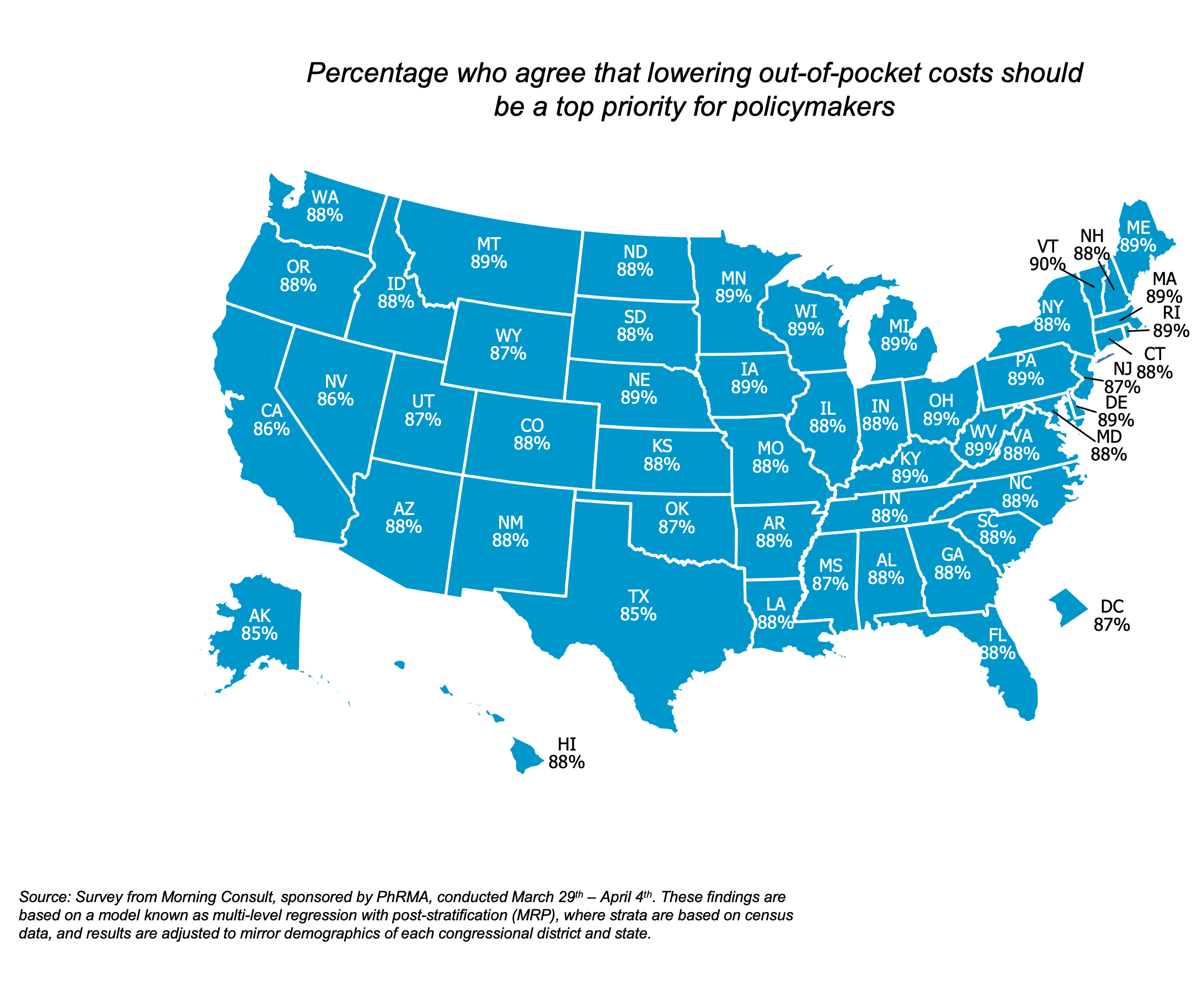
88% of American adults across all 50 states agree that policymakers should prioritize lowering their out-of-pocket health care costs. When given two options, over 50% of those surveyed would rather see the out-of-pocket costs decrease rather than pay a lower monthly premium.
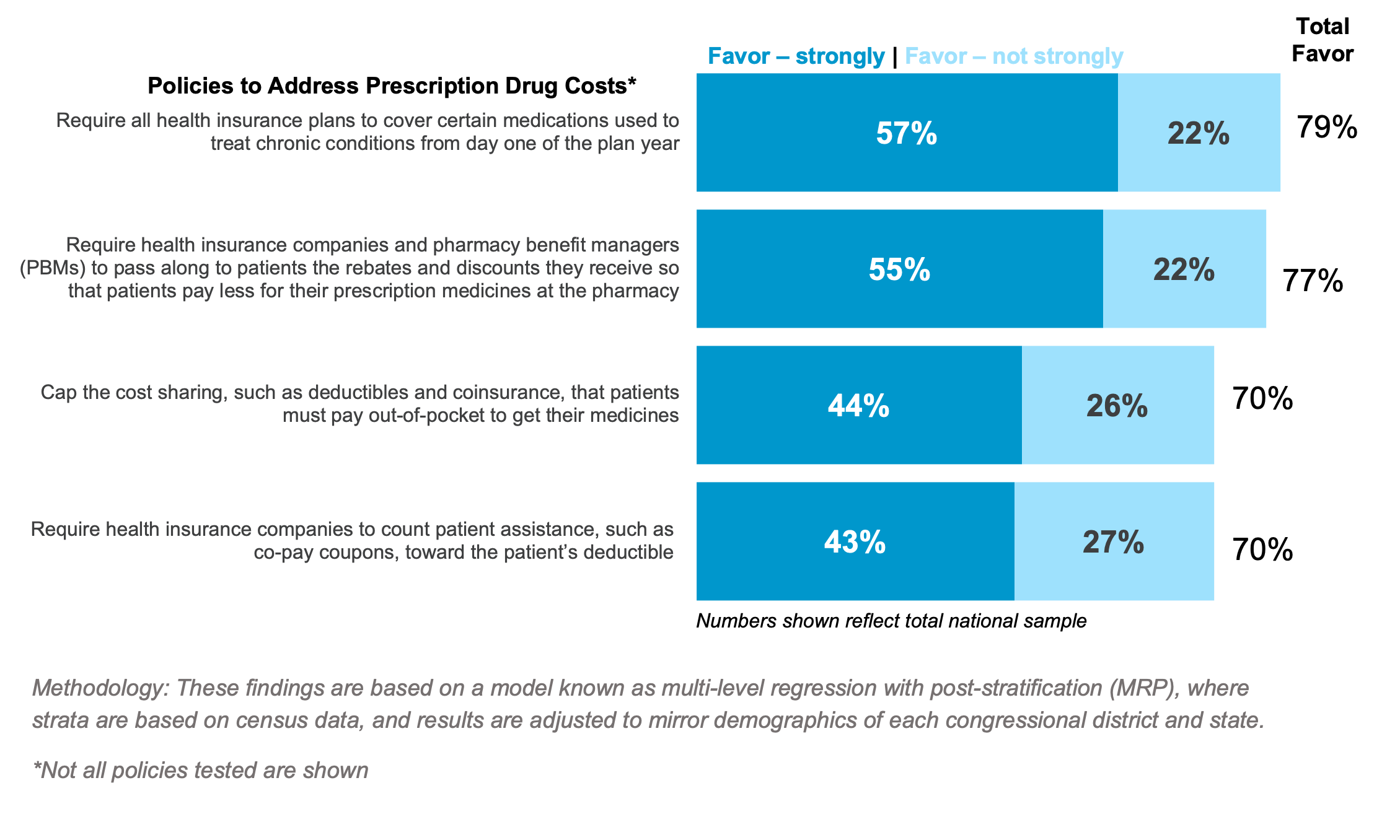
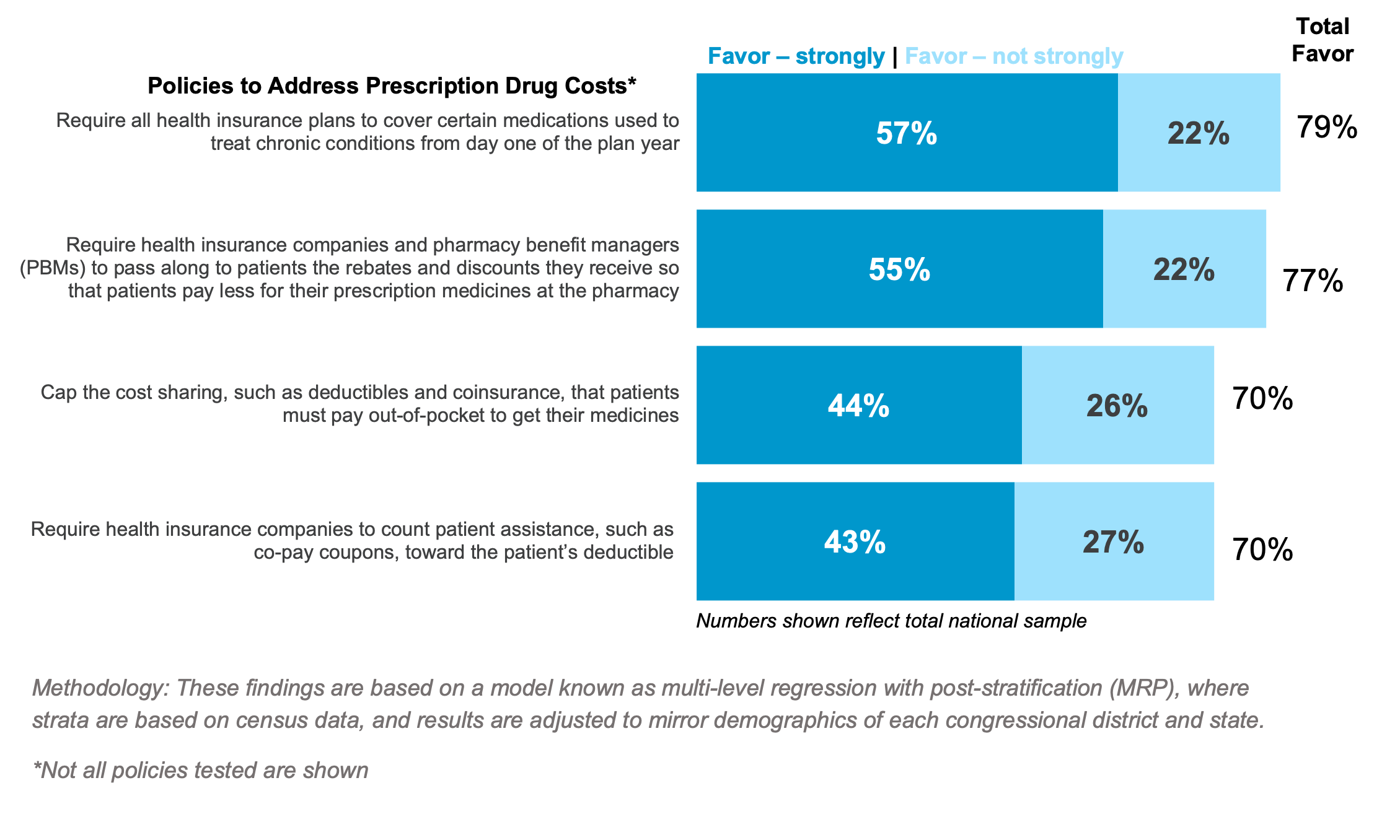
When it comes to bringing actual solutions to the table, 77% of those surveyed favor requiring health insurance companies and pharmacy benefit managers (PBMs) to share the savings they receive directly with patients at the pharmacy counter.
Insurance companies and their PBMs often require patients to pay either the full list price of their medicine or set patient cost-sharing based off the full list price of the medicine. Policies at the state level to address this could save some patients nearly $1,000 annually on their medicines.
On the other hand, there could be very damaging effects of taking the wrong approach through drug price setting policies — including leaving the accessibility and affordability of prescription medicines in the hands of unelected officials or partisan politics. Over half of adults oppose drug price setting policies, such as prescription drug affordability boards, once they learn more about the policy and are presented with tradeoffs, such as:
- “It could limit people’s access to newer prescription medicines” (57% oppose)
- “Patients could have reduced access to fewer prescription medicines” (57% oppose)
- “It could take away power from doctors to prescribe medicines that best meet the needs of their patients” (56% oppose)
When patients visit their doctors, it’s staggering to hear about how big of a bind they are in when it comes to ensuring the medicines they are prescribed are the ones they can afford and access. Together, we have the very real opportunity to bring relief to one area of great financial and, most importantly, personal need.
It’s time to put people over the bottom line. States can require PBMs, insurers and other middlemen to put patients first.
To stay up to date with PhRMA’s state policy findings and information, visit www.PhRMA.org/States.
This poll was conducted by Morning Consult, on behalf of PhRMA between March 29 – April 4, 2022, among a national sample of 20,000 adults. These findings are based on a model known as multi-level regression with post-stratification (MRP), where strata are based on census data, and results are adjusted to mirror demographics of each congressional district and state.