A recent congressional forum looked at the role pharmacy benefit managers (PBMs) play in determining what patients pay out of pocket for prescription medicines. The forum provided an important reminder of how these middlemen operate in an opaque system that often leaves patients paying far more than they should for medicines. And it’s also a reminder of what’s missing from the current drug pricing bill that passed in the House last week:
PBMs and the health plans they work for are receiving a greater share of spending on prescription medicines. Drug companies set list prices for medicines and then negotiate rebates and discounts with PBMs to help ensure patients have access to them.
Patients too often DO NOT benefit from these rebates and discounts when they go to the pharmacy.
- Patients with deductibles often pay based on the undiscounted list price of a medicine while their health plans can pay nothing and still receive a rebate. In fact, half of commercially insured patients’ out-of-pocket spending is based on the full list price.
- Forcing patients with deductibles and coinsurance to pay based on the undiscounted list price of a medicine only happens with medicines – out-of-pocket expenses for other health care services are tied to the lower, negotiated price paid for those services.
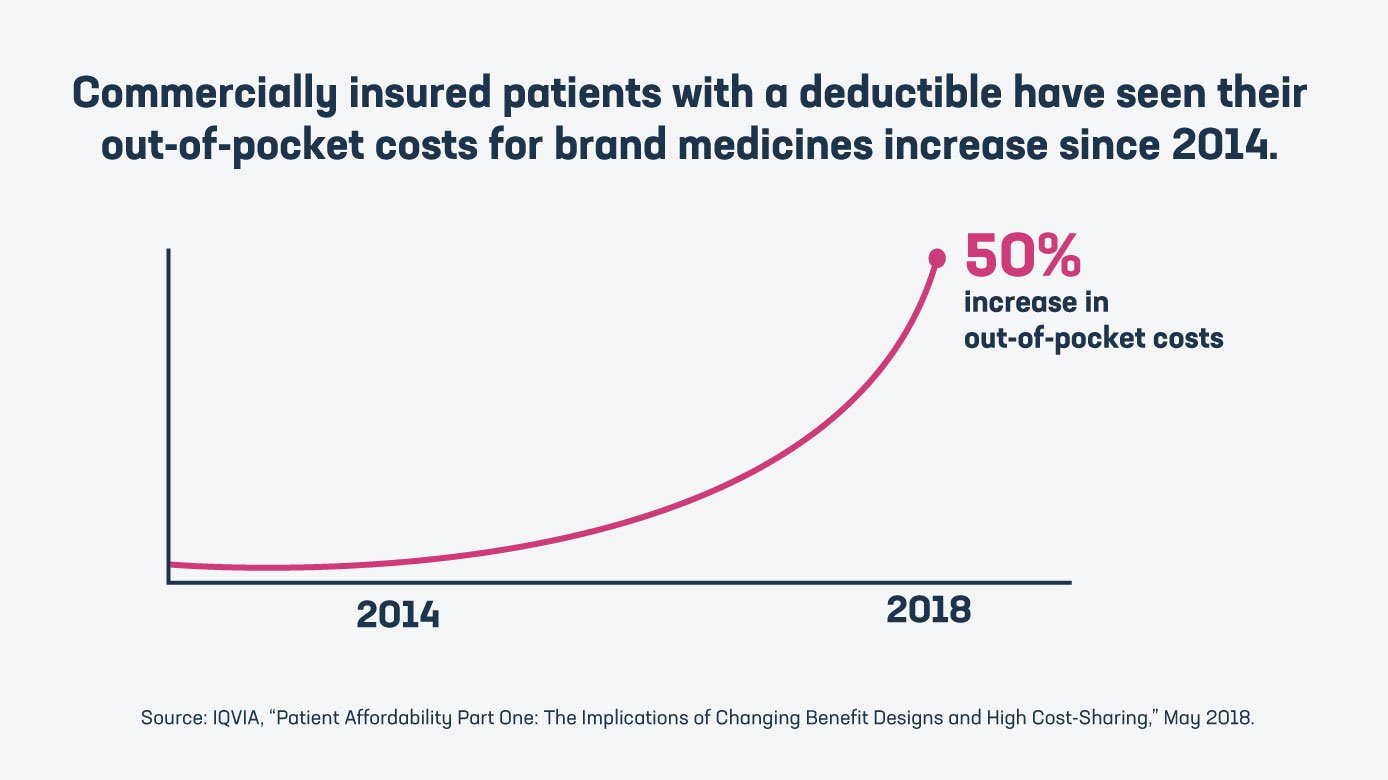
- Commercially insured patients with a deductible have seen their out-of-pocket costs for brand medicines increase 50% since 2014. In addition, half of patients with a high deductible reported trouble taking their medicine as prescribed by a doctor.
- The system we have today, as described by the experts at 46 Brooklyn, is one that takes “money from sick people” to subsidize the care of healthy people.
Sharing savings directly with patients at the pharmacy would help fix perverse incentives in the system and lower out-of-pocket costs.
Unfortunately, the drug pricing bill currently being debated in Congress does not meaningfully address these concerns. The bill:
- Does not bring the kind of accountability and transparency to PBMs that patients and employers need.
- Does not address a broken insurance system that is shifting more of the costs of medicines onto vulnerable patients.
- Does not take steps to ensure patients share in the savings PBMs and health plans receive.
[The drug pricing bill] doesn't address perverse incentives in the system that are leading to higher costs for patients.
Stephen Ubl, PhRMA President and CEO
Instead of a drug pricing bill that helps address the real affordability challenges facing patients, we have a bill that PhRMA President and CEO Stephen Ubl has said “doesn’t address perverse incentives in the system that are leading to higher costs for patients.” That is why Ubl has called on Congress to reject this flawed bill and “instead work to advance commonsense, patient-centered solutions that we know enjoy bipartisan support.”
Learn more at PhRMA.org/BetterWay.




 Sharing savings directly with patients at the pharmacy would help fix perverse incentives in the system and lower out-of-pocket costs.
Sharing savings directly with patients at the pharmacy would help fix perverse incentives in the system and lower out-of-pocket costs.

