This morning at the National Press Club, PhRMA CEO John J. Castellani joined patient groups to release new research from Avalere Health.
Following reports that patients with health insurance exchange coverage face high deductibles and high-out-of pocket costs for prescription medicines and that even when cost-sharing reductions are available they’re doing little to help with prescription access, this new research finds that many plans are placing all medicines in at least one class on the highest cost-sharing tier, including, in some cases, generics.
Some key findings:
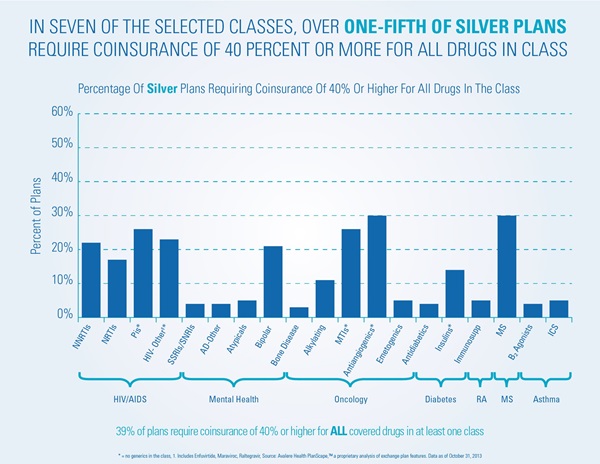
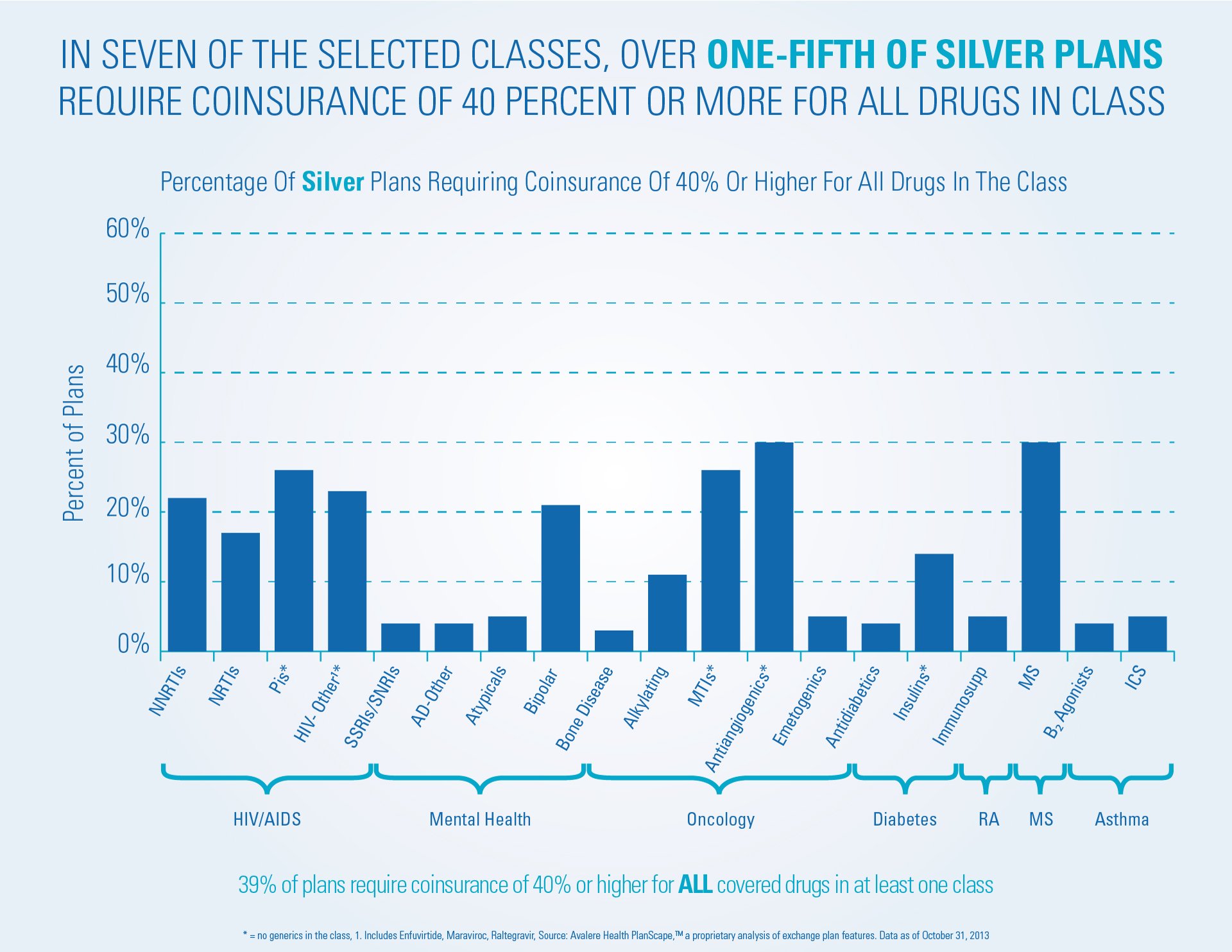
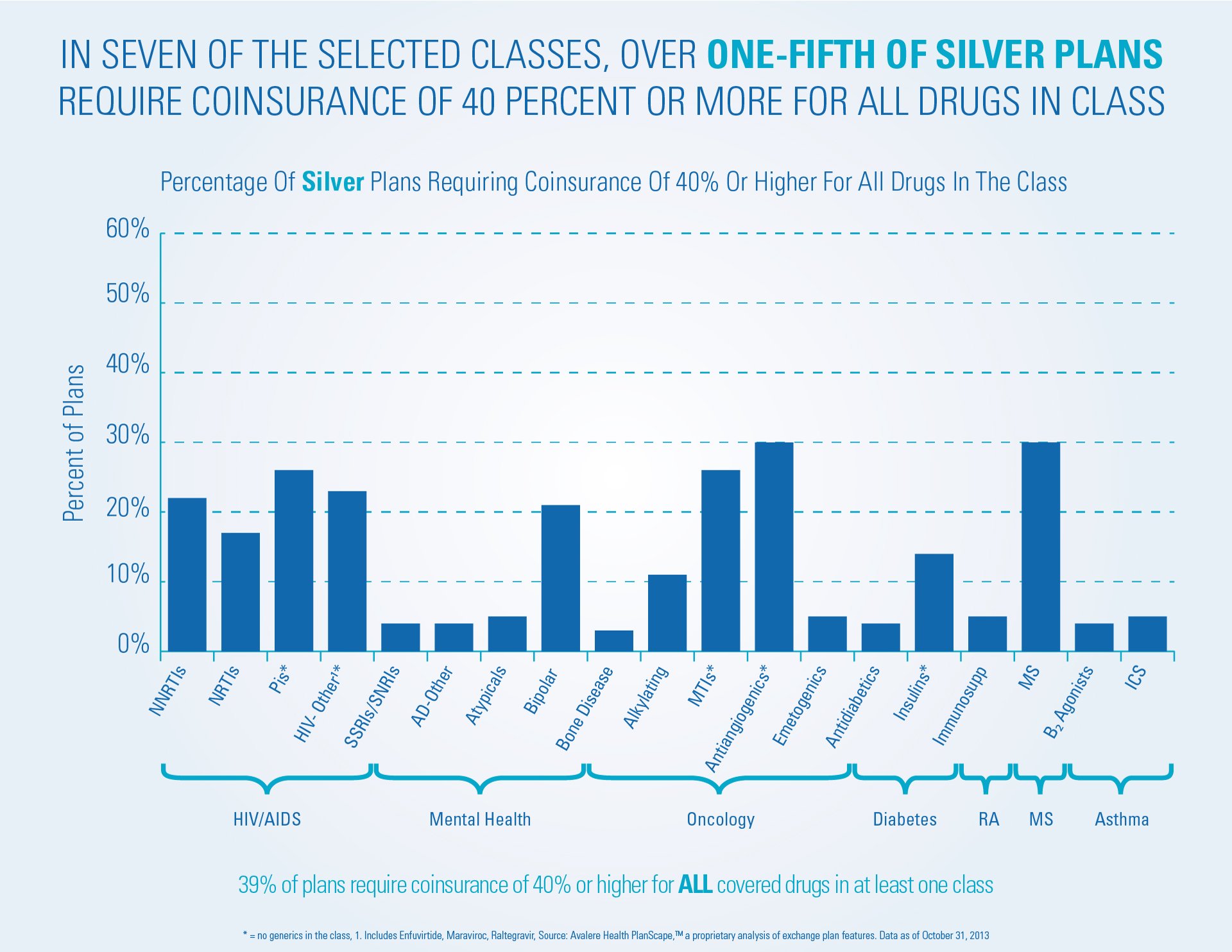
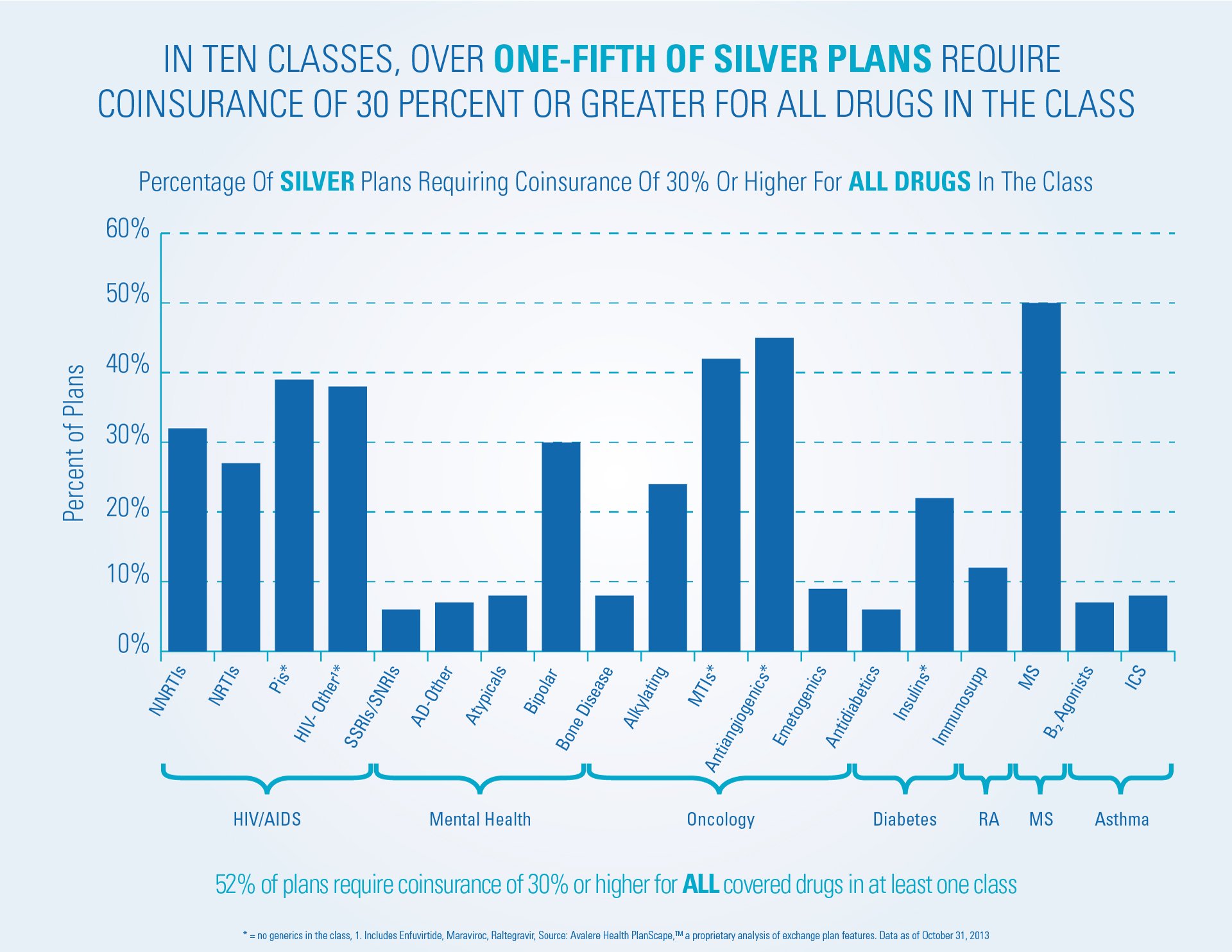
- In seven classes of medicines treating serious illnesses like cancer, HIV/AIDS or multiple sclerosis, more than 20 percent of Silver plans require coinsurance of 40 percent or more for ALL medicines in the class.
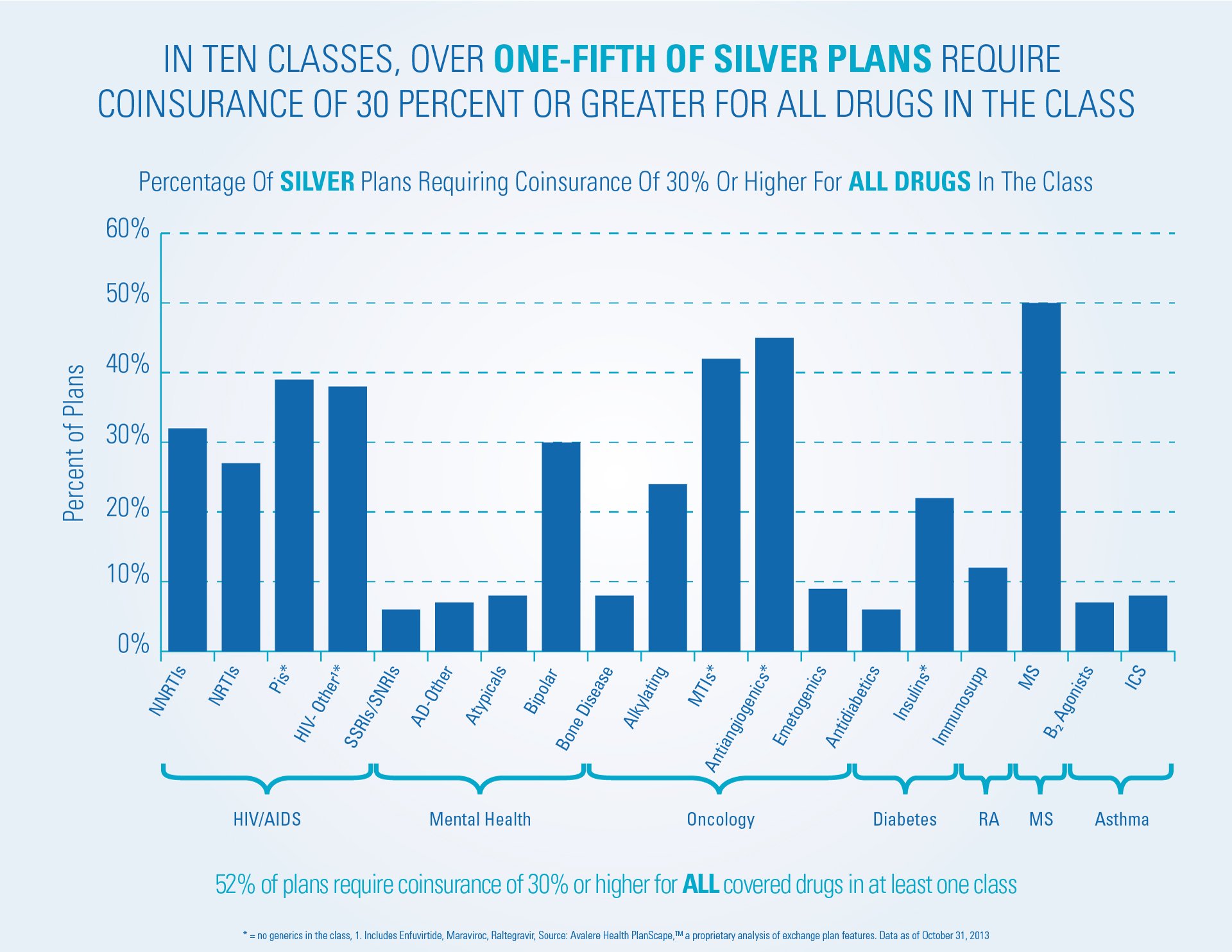
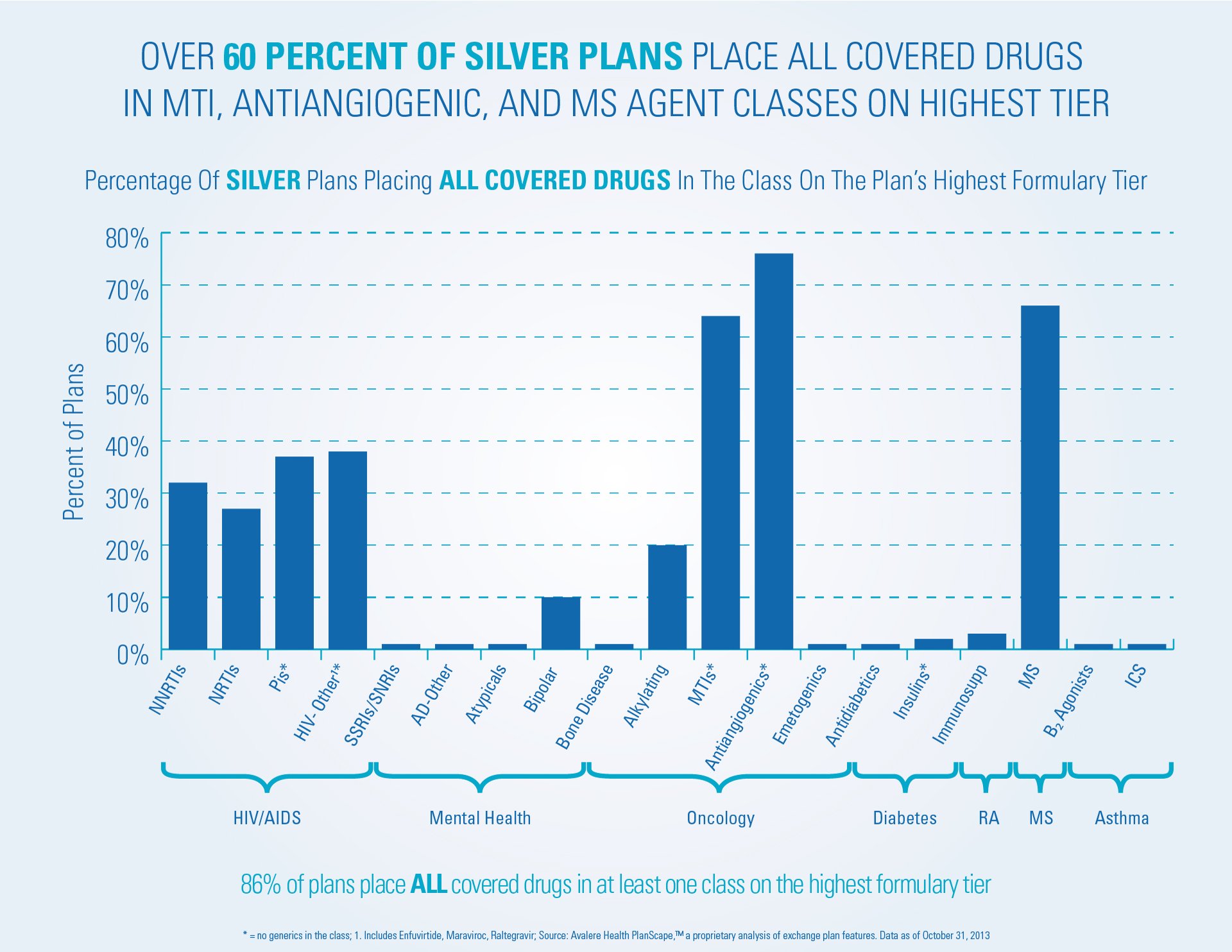
- More than 60 percent of Silver plans place all covered medicines in the class for treating MS on the highest cost-sharing tier.
- More than 60 percent of Silver plans place all covered medicines for treating certain types of cancer on the highest cost-sharing tier.
- Almost all Silver plans (86 percent) place all medicines in at least one class on the highest cost-sharing tier.
Patient groups, including those representing patients with HIV/AIDS, cancer, autoimmune diseases, and immune deficiencies, echoed the findings of the report and shared stories of patients being forced to forego their needed treatments.
New, innovative, and lifesaving medicines are critical to patients managing these conditions. When patients adhere to their medications, their quality of life is better, health outcomes improve, and health care costs overall go down. But when insurance plans place all needed medicines to treat these conditions out of reach, patients suffer.
The Affordable Care Act is supposed to provide Americans – including those with serious medical conditions – the opportunity to purchase meaningful and affordable health insurance. This report is evidence that for many, that opportunity has not been realized. Now is the time to address the serious obstacles patients with health insurance exchange coverage are facing.