Critics proven wrong again on medicine spending
Recent comments from payers disprove – once again – the fallacious claims previously made about spending on new medicines.
Critics proven wrong again on medicine spending
Recent comments from payers disprove – once again – the fallacious claims previously made about spending on new medicines.
Critics proven wrong again on medicine spending
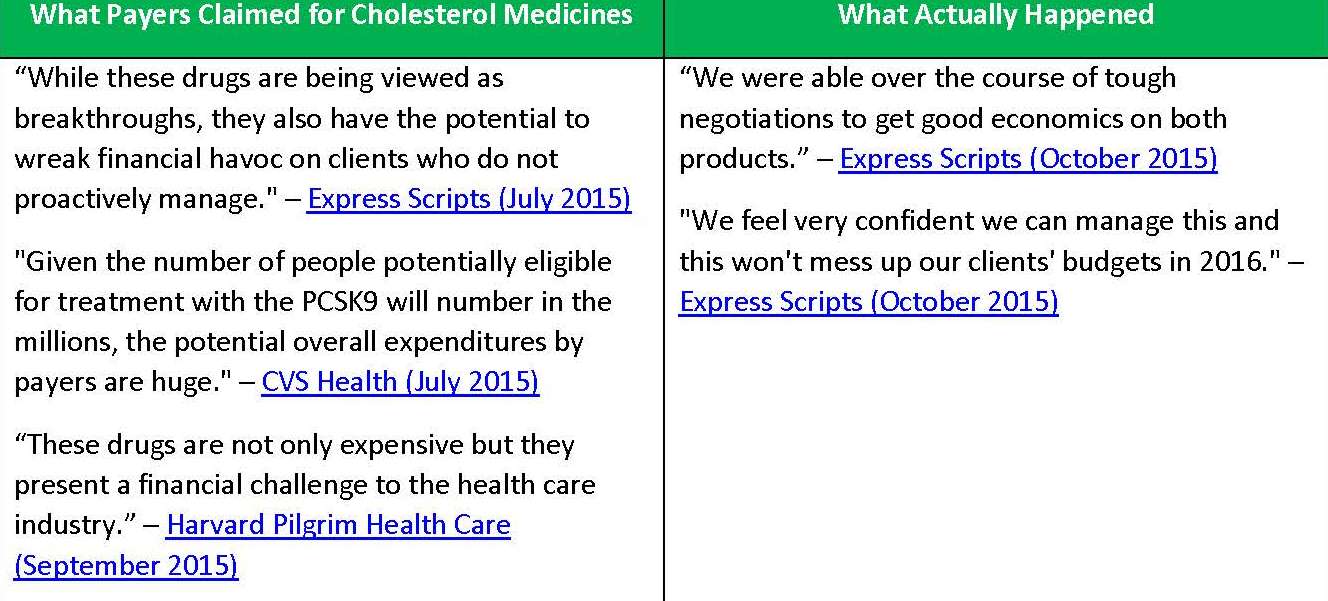
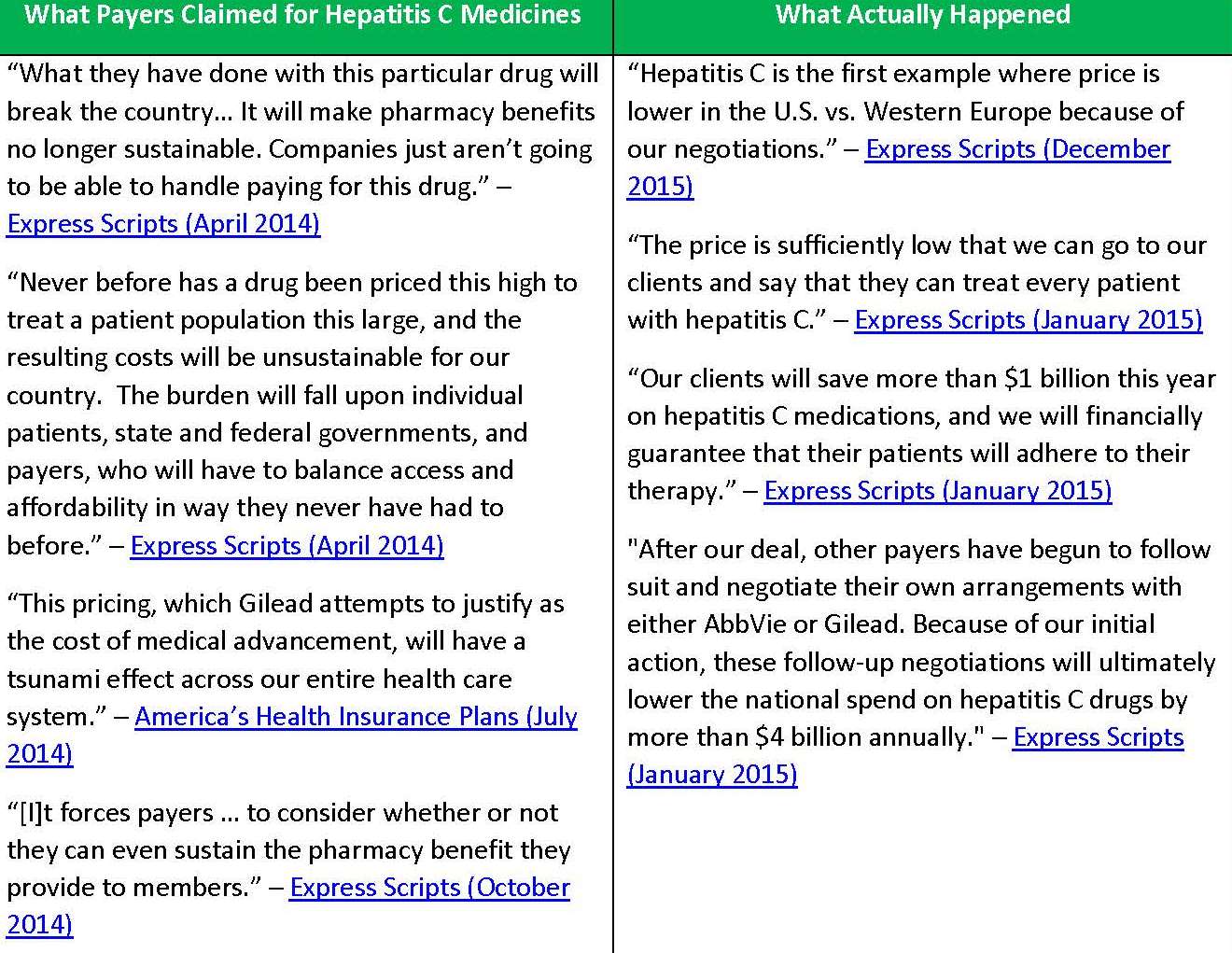
Recent comments from pharmacy benefit managers and insurers disprove – once again – the fallacious claims previously made about spending on new innovative medicines. Over the past year, payers claimed life-changing treatments and cures for hepatitis C and high cholesterol would bankrupt the health care system and wreak financial havoc.
Yet just last week, Express Scripts, the largest pharmacy benefits manager in the U.S., proudly tweeted “Hepatitis C is the first example where price is lower in the U.S. vs. Western Europe because of our negotiations.” And in October, they touted they can include both new cholesterol-lowering medicines, called PCSK9 inhibitors, on its national list of covered medicines thanks in part to
substantial – and typical – discounts negotiated.
These statements undermine the claims Express Scripts and other payers made that new medicines would force them to consider whether or not they can even sustain the pharmacy benefit they provide to their members.
Why were they so wrong?
Because our nation’s competitive marketplace works to control costs while encouraging the development of new therapies that help patients live longer, healthier lives.
Conversations about costs are important, but we need to put doomsday predictions in context. Focusing solely on the share of spending that goes toward life-changing medicines will not solve our nation’s health care challenges. Instead we need to find solutions that ensure access to high quality, patient-centered care and continue to encourage development of innovative medicines.
Here is a sampling of the egregious claims payers made and what actually happened.
Read more about the cost and value of medicines at www.phrma.org/cost.