Americans with mental health conditions often have to deal with stigmas surrounding their illness and other social barriers that have the potential to limit their access to care. This morning the U.S. Health and Human Services Department announced several parity rules are set to take effect to help eliminate the disparity in care for patients with mental illnesses versus patients with physical ailments. Proper care and treatment is critical to mental health patients as well as their friends and families.
Mental health conditions affect 1 in 4 Americans and more than 450 million people worldwide - they’re our friends, neighbors and loved ones. Early and effective treatment is critical to helping these individuals. And clinicians often base their treatment selections on highly individualized factors in an effort to help patients in the most effective way.
Kay Jamison, for example, noted how her severe form of bipolar disorder left her “without hope and … without any sense that you can deal with the future and deal with your life,” but thanks to the treatments available, she has been able to lead a “very good life” as a professor in the Department of Psychiatry at Johns Hopkins School of Medicine. Elyn Saks, a law professor at the University of Southern California, also underscored the importance of effective medicines, noting that excellent, consistent treatment helps her live with schizophrenia.
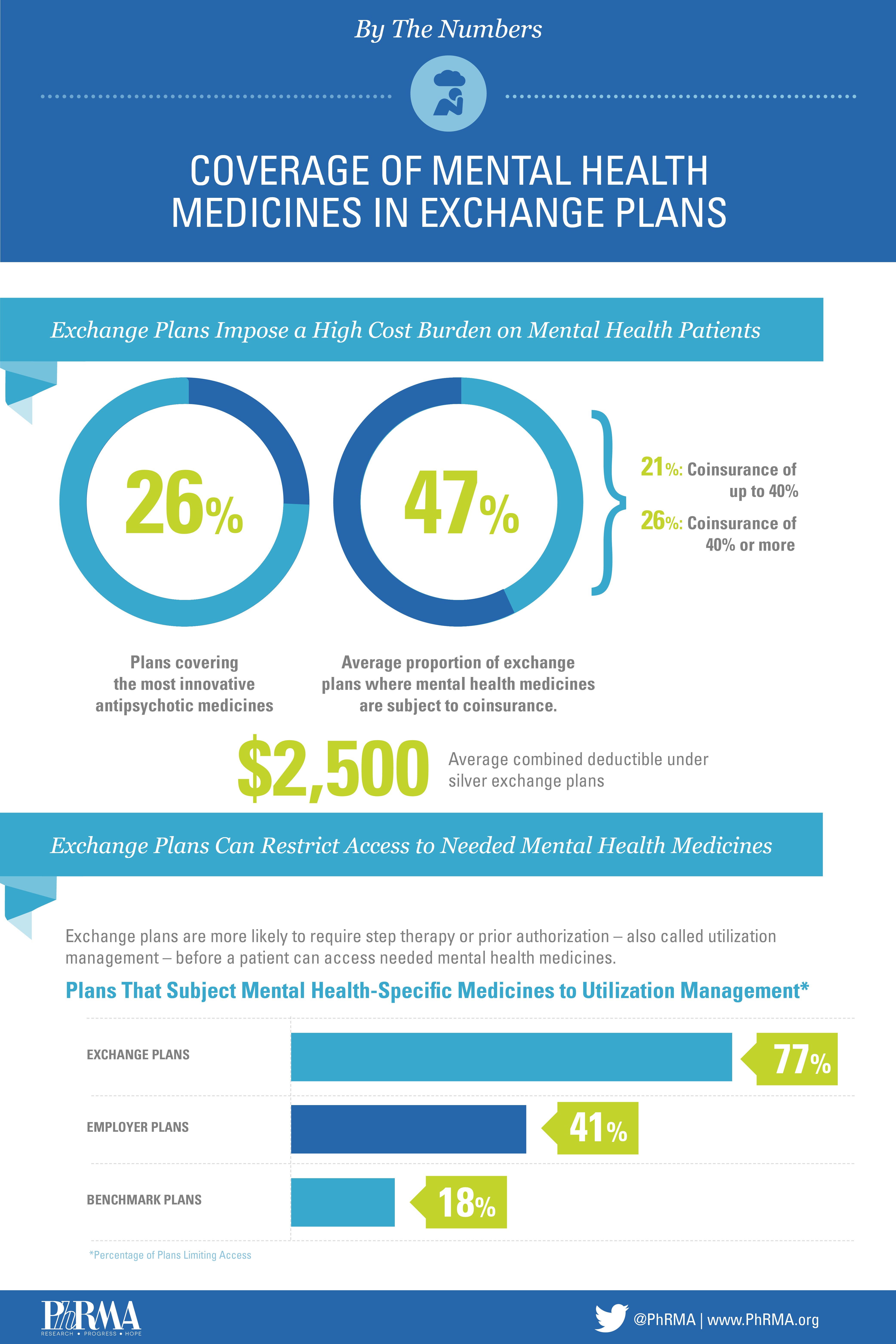
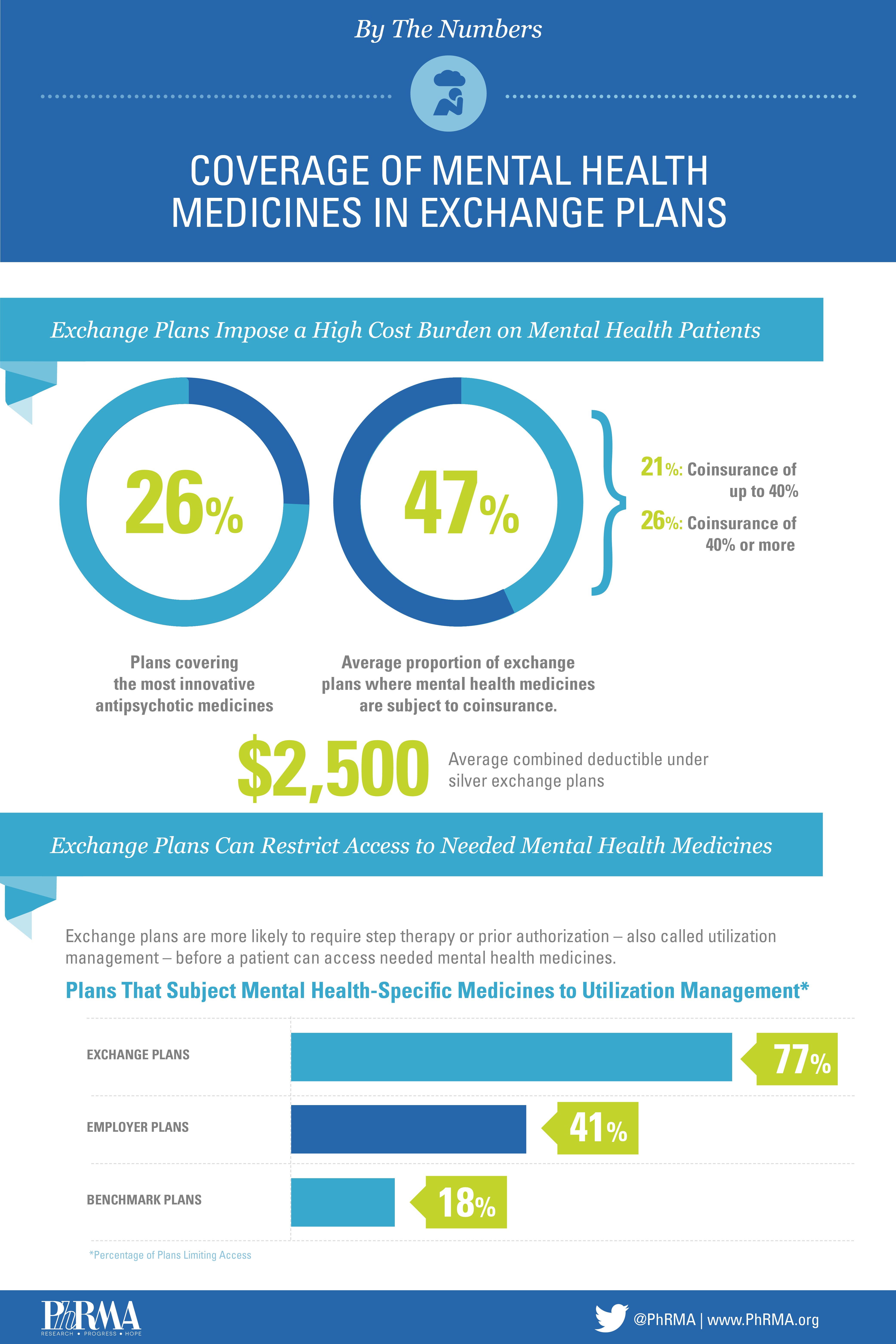
These individuals had access to the individualized treatments they needed, but what if a patients’ ability to get necessary medicines is jeopardized? The health insurance exchanges implemented as part of the Affordable Care Act are designed to eliminate barriers to access and help patients get the treatments they need, but research suggests this may not be the case. The plans fail to cover some types of necessary medicines, and as a result, patients and the health care system are at a disadvantage.
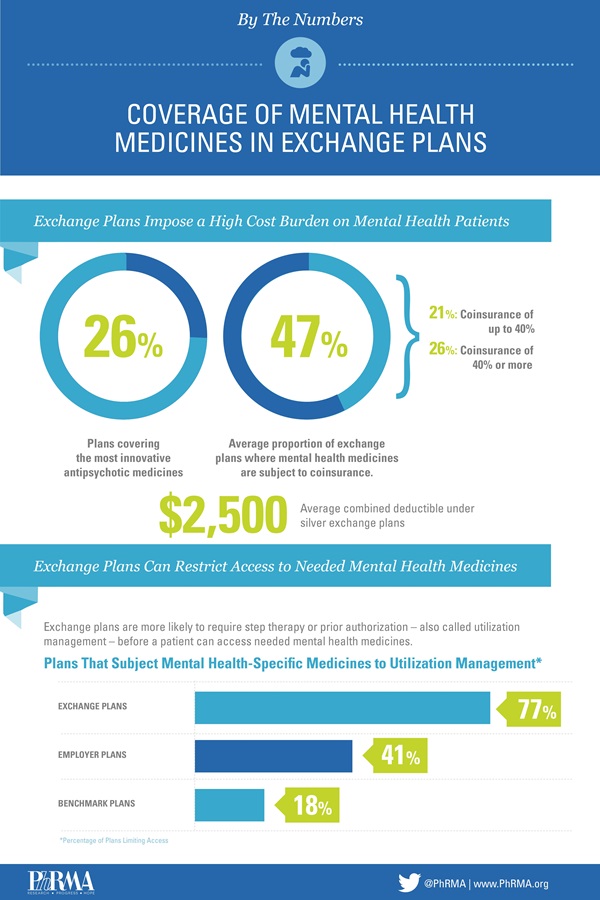
Just 26 percent of the most innovative antipsychotic medicines, for example, are covered by exchange plans and those without a generic equivalent are also frequently excluded. This is troublesome given the complexities of treating mental health conditions. Fast-acting formularies are often critical to quickly stabilizing a patient to ensure their safety and the safety of others, and long-term, injectable medicines may be necessary to improve adherence and help an individual’s overall well-being. These treatments, however, are covered at just 58 percent and 17 percent, respectively on exchange plans.
What’s more, many of these plans force patients to pay a lot out-of-pocket, which increases health care costs for patients and the broader health care system. Nearly one in two Silver health insurance exchange plans subject mental health medicines to coinsurance; on one in four plans, that coinsurance is 40 percent or more. Research shows that the more an individual must pay for medicines, the more likely they are to forgo treatment, leading to more costly acute care. Exchanges also tend to apply a global deductible for both medicines and other services for patients with mental health conditions, which means they have to pay an average of $2,500 in silver plans and $4,300 in bronze plans out-of-pocket before any coverage for treatment is offered.
Mental health conditions affect individuals regardless of race, gender or socioeconomic status, but by failing to adequately cover the medicines patients need and forcing individuals to pay more out-of-pocket, we are only hurting these patients.
Affordable coverage and access to a range of mental health medicines is critical to meeting patient needs. For more on the current state-of-affairs for mental health innovation and what we need to do to ensure patients have access to the best possible treatment options, we encourage you to read about our Mental Health Capitol Hill briefing held last week.
As we continue to explore what exchanges coverage means for individuals with mental health disorders and other chronic conditions, we encourage you to follow us on The Catalyst, Twitter and Facebook for more information.