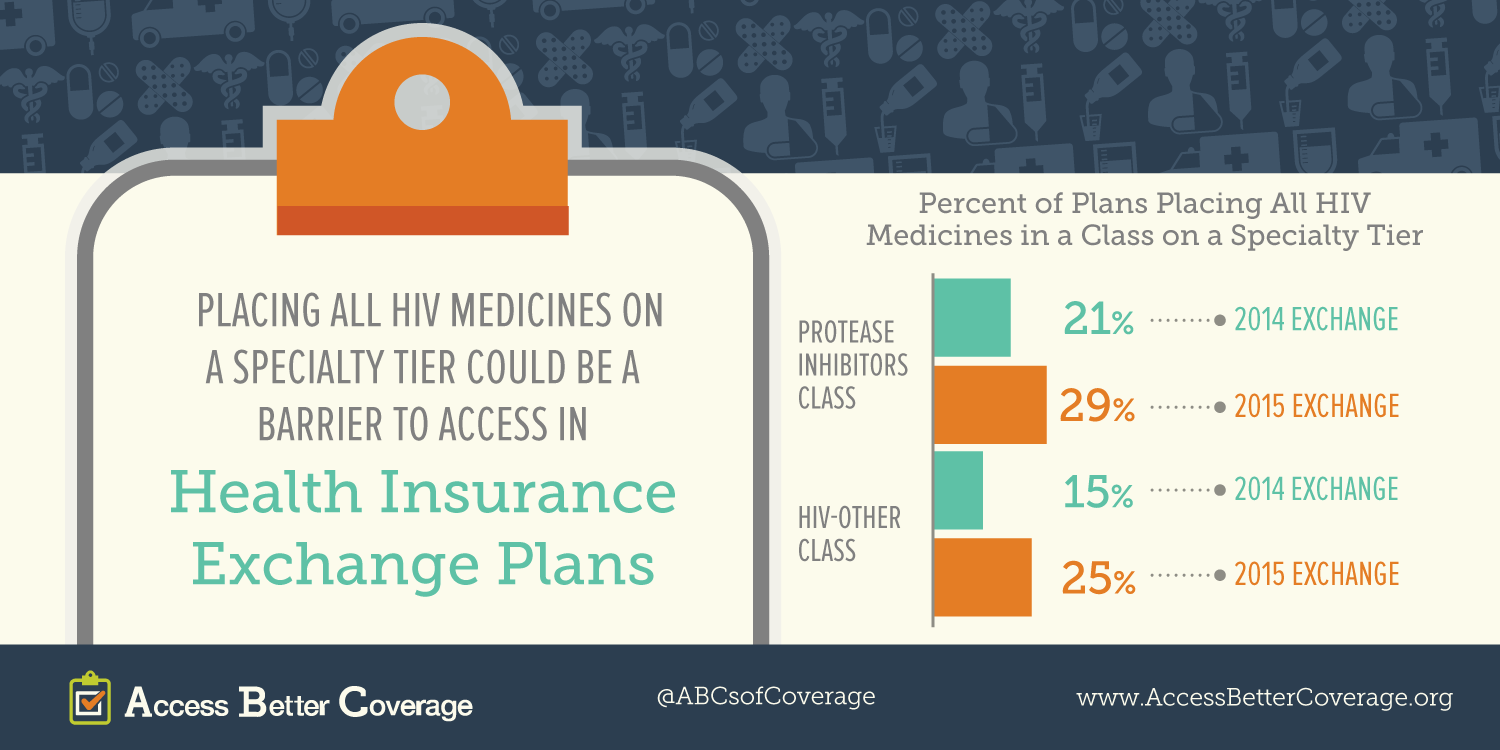
Patients, especially those suffering from chronic conditions, deserve access to the medicines they need to live longer, healthier lives. Today, PhRMA released a new fact sheet on access to HIV/AIDS medicines in exchange plans in 2015 (2014 fact sheet is available here). The fact sheet highlights some of the potential barriers to accessing needed treatments. Learn more on AccessBetterCoverage.org, in our patient profiles and our other fact sheets.
This is the second post in our Burden on Patients Q&A series with patient advocates. To learn more, we talked with Carl Schmid, deputy executive director for The AIDS Institute.
Question (Allyson Funk): What is the AIDS Institute and who do you represent?
Answer (Carl Schmid): We’re a national public policy and advocacy organization with a focus on HIV and hepatitis issues. We were founded in Florida and still maintain our presence there, and we have our national policy office in Washington, D.C. Our goal is to make sure people with HIV and hepatitis are given the proper care and treatment they need as well as prevent new infections.
Q: How do medicines help patients manage HIV/AIDS?
A: In the 1990s, the pharmaceutical industry began to develop medications that not only treated infections caused by AIDS, but also drugs to slow or block replication of the virus. Back then patients would have to take 10 or 20 pills (or more) a day. But today, highly active antiretroviral treatments combine multiple drugs into one pill, dramatically reducing the pill burden for patients and extending life expectancy of people living with HIV.
Most people with HIV can live a long life if they have access and adhere to their medications. Treatment does have its side effects and does not always work for everyone, so continued medical innovation is needed. We now know that treatment not only prolongs the lives of people living with HIV, but by reducing a person’s viral load, treatment acts as prevention as well.
[Note: Carl recently answered this question in-depth in our Conversation on the Anniversary of the Ryan White Care Act. Read his full response here.]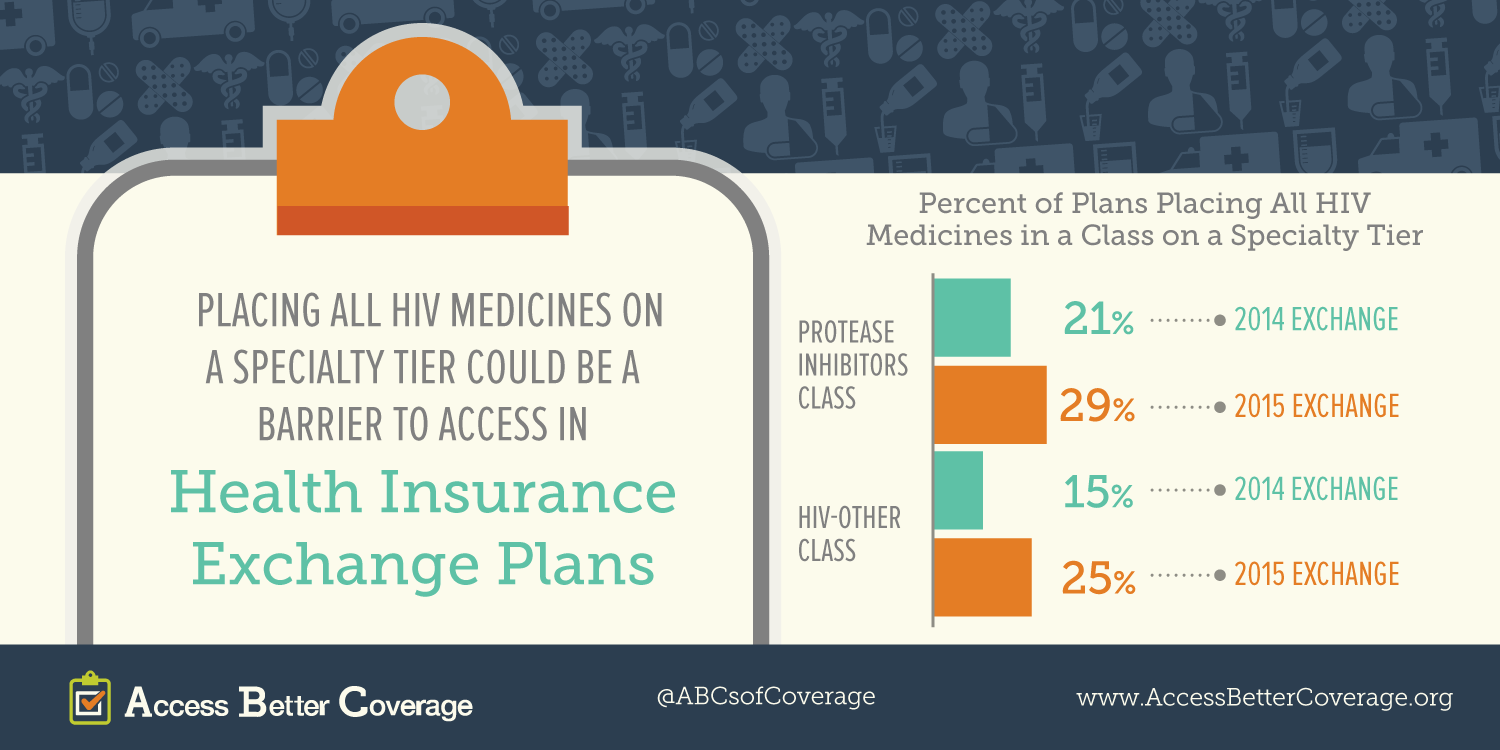
Q: The Affordable Care Act (ACA) expanded health insurance coverage to a broader population. What are you hearing about coverage in health insurance exchanges, in particular access to HIV/AIDS medications?
A: On the whole, many of the drugs are on the formulary. For many people, if they choose the right plan can access the medications at a reasonable price. The issue is if you choose the wrong plan you may face a very high deductible before you can access the medications or the drugs may not be on the formulary. We’re finding that many of the newer treatments aren’t on some plans and often there are a lot of HIV medications on the highest tier. This is not in all plans, but in some plans. In fact, some plans are putting all of the HIV drugs on the highest tier.
And instead of charging copays, some plans are charging coinsurance of 30, 40 or 50 percent which could mean an out-of-pocket cost to the patient of over $1,000. That’s what we’re finding as a problem. What the Avalere data has shown is that this is a growing trend. More plans are putting HIV drugs on the highest tier and charging coinsurance.
Q: What are the biggest concerns facing HIV/AIDS patients in health exchanges?
A: It’s the coinsurance and the high out-of-pocket cost sharing patients are encountering. This is really dangerous because HIV patients need access to their medications every single day.
We hear stories about people going into the pharmacy and picking up their drugs for the first time and they are shocked because they didn’t know what 50 percent coinsurance was. As a result, they might not pick up their medication and that’s dangerous for their health and well-being.
One other issue with coinsurance is that there is no transparency. No one knows the true patient cost-sharing up front since they do not know what 30 percent or 40 percent translates into in terms of dollars. Patients need to have that information so they can select a plan that meets their needs.
Q: Is there anything else we missed?
A: We’re also seeing quantity limits and prior authorization for HIV drugs. That’s also dangerous for patients. Limiting patient access to the prescriptions their providers are prescribing for them.
HIV is very unique and every patient has different needs. They could be resistant to a medication or there could be side effects from a medication or may have other diseases. It’s important patients be able to get the medications their provider prescribes.